
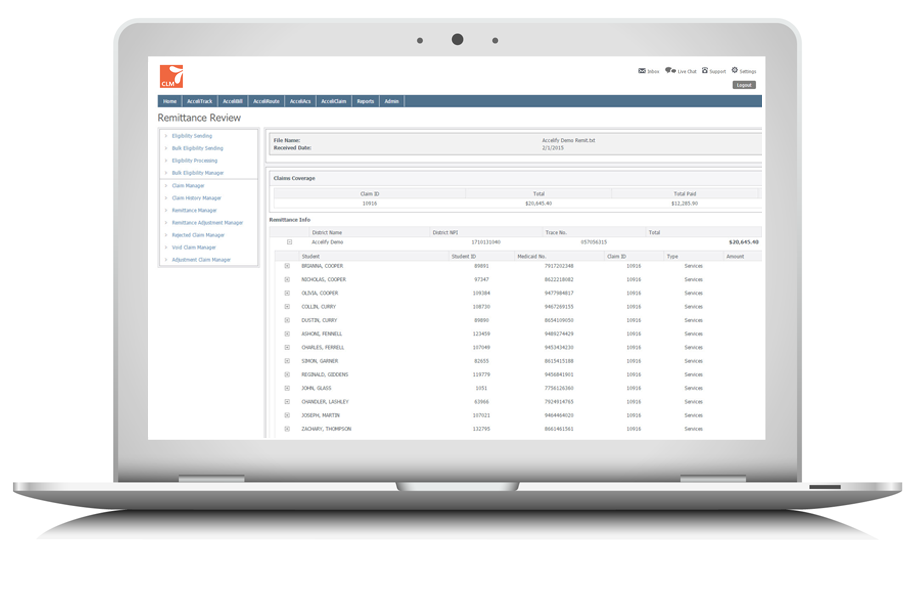
AcceliCLAIM manages every step of the Medicaid claiming process, from performing Medicaid eligibility checks, to building and submitting claims, to processing remittance files. The system performs complex validation routines to ensure only eligible services are claimed and includes a suite of reporting tools designed to help you identify where additional data can drive greater reimbursement.
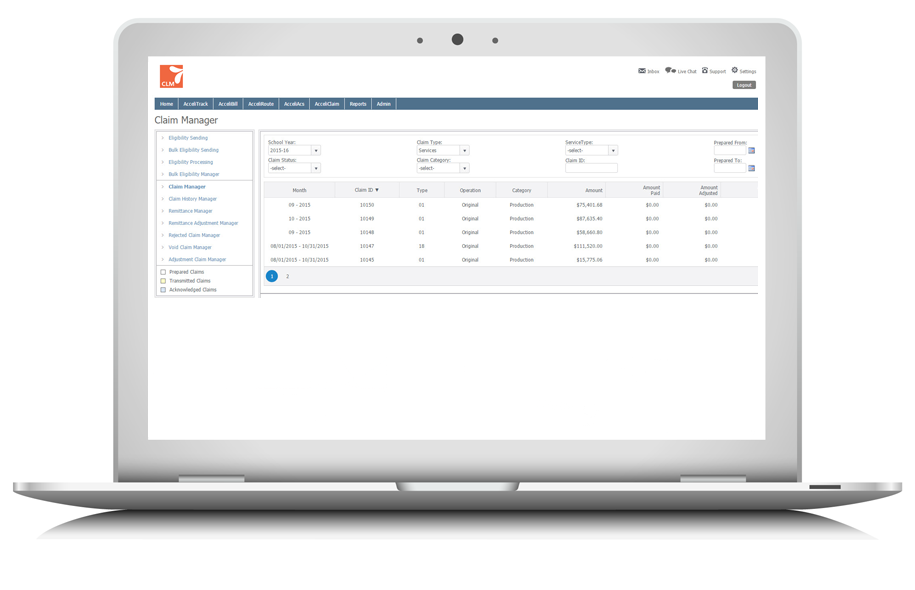
AcceliCLAIM provides visibility into every stage of the Medicaid claiming process. From student eligibility to services claimed and payment information, the system provides detail down to the “line item” level, so you can see which students and services are (and aren’t) being claimed and paid. When services are denied, the system displays the reason why, and provides the ability to instantly correct, adjust and resubmit the claim electronically, so you can ensure every eligible service is paid.
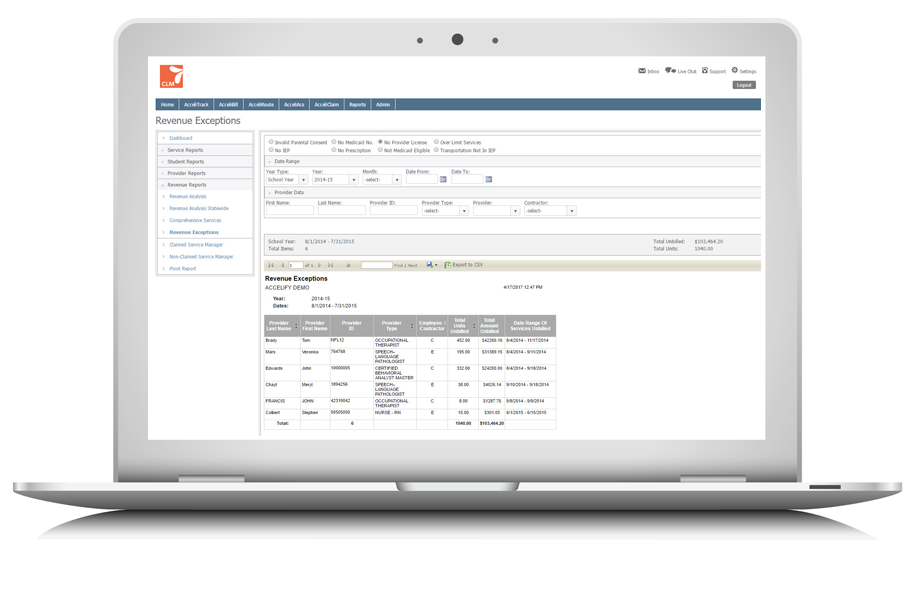
AcceliCLAIM reports when potentially eligible student services are missing data (like parental consent or provider licensure information), including the dollar value of each non-claimed service, allowing you to target your efforts at obtaining missing information for those students and providers with the greatest revenue tied to them.
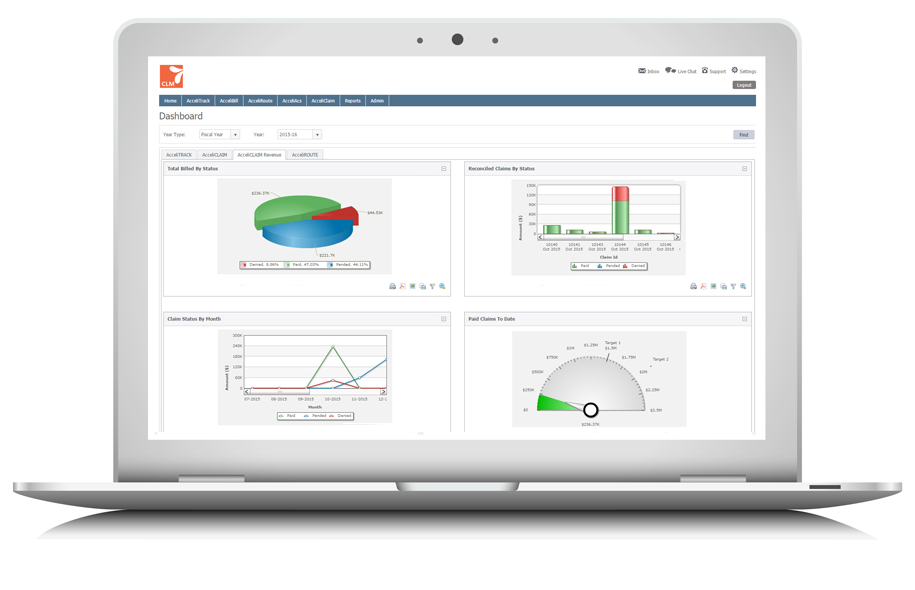
The AcceliCLAIM reporting suite includes dashboards that provide instant access to eligibility trends, the status of claims (pending, paid, denied), and allows you to pivot revenue data by claim, provider type, school building, and more.
IEP authorization, physician prescriptions, parental consent, provider NPIs, provider license dates, service records, Medicaid eligibility, student information. As this list suggests, collecting and maintaining the required data to prepare compliant Medicaid claims can be cumbersome. AcceliCLAIM eases the process by linking directly with the source of each data element (e.g. SIS, IEP) and automatically performs a complex set of validation routines to ensure only eligible services are claimed. AcceliCLAIM also ensures this data is readily accessible to defend your district in the case of a Medicaid audit.